This is sourced from the appendix of Bone Stimulus: Summary and Applications, click here to read the full whitepaper.
Different types of bone
Our bones consist of two functionally different types. Spongy bone, also known as cancellous or trabecular bone, is the type of bone that you find at the ends of a long bone and the center of our spine. The spongy bone is where red blood cells are made (we produce 2.4 million new red blood cells each second! In fact, a quarter of the cells in your body are red blood cells!). Compact or cortical bone is the dense bone you find at the shaft of a long bone, and the surrounding outer shell of the bone. It is responsible for providing structural strength to bone and makes up 80% of skeletal mass.
Bone modeling vs bone remodeling
There are two important processes to consider when thinking about how bone adapts and changes to the mechanical environment. One process is bone modeling
. This is the process by which new bone is formed during growth and development (i.e. until the skeleton is mature, around age 19 or 20 yrs). The second process is bone remodeling
. This is the continued adaptation and regulation of bone after skeletal maturity (i.e. adaptations of the adult skeleton).
What is bone remodeling?
Bone remodeling is a tightly regulated process of repairing microdamage and replacement of old bone with new bone. Remodeling occurs through the breakdown (resorption) of old bone with the formation of new bone. The rate of remodeling is regulated by biological factors (hormones, age, etc) and the mechanical environment.
How do the bone cells actually remodel the bone?
In cancellous (spongy) bone, remodeling occurs on the surface of trabeculae (miniature struts) and lasts about 200 days in normal bone. The first step in this process involves resorption of a small tunnel (lacuna) by cells called osteoclasts. This resorption has a median duration of 30-40 days. Following resorption, these microscopic (40-60 micron in length) tunnels are filled with new bone by cells called osteoblasts. This process takes ~150 days. The total surface of cancellous bone is completely remodeled over a period of 2 years. In disease states, such as osteoporosis, the osteoblast cells are unable to completely fill the resorption lucuna, resulting in a net loss of bone. The remodeling process of cortical bone occurs in only 120 days.
How does mechanical loading influence bone remodeling?
Certain athletic activities (or an increase in body weight) can promote bone formation. Severe bone resorption will occur through inactivity or bed rest (i.e bone responds more to inactivity than increased activity, which is bad news for astronauts wanting to travel to Mars!). The number of loading cycles, as well as the stress magnitudes, influence skeletal mass. Bone responds more to a high strain rate (i.e. larger forces over a shorter time), compared to the number of cycles. The consequence of this is that bone can respond the same way to exercise that is high force-low cycle or medium force-high cycle. For example, animal studies have shown that a 40%
increase in bone mineral density in the mid-shaft of the rooster ulna occurred after only 36 cycles per day at physiologic strain levels. Increasing the number of loading cycles to 1800 per day had no additional observable effect on bone mineral density. This explains why a marathon runner does not have a bone mineral density that is 50x more dense than you or I, even though they might experience 50x more cycles of loading!
Can adults increase bone mineral density by changing our physical activity levels?
Only modest gains in bone density have been achieved in adults with mild exercise added as a supplement to normal daily activity. The amount of new bone formation is not only a function of your daily activity, but also depends on the load history of the bone. For example, an athlete who is already a trained runner will have very little increase in bone formation if they add some extra miles into their training schedule. However, a sedentary individual who experiences that same mileage might experience a greater response in bone formation. Across the general healthy population, we see fairly modest differences in bone density. For example, measurement of the calcaneal (heel) bone indicates ~20% difference in bone mineral density between cross-country runners and a control population of non-runners.
Does bone mineral density determine the strength of the bone, and hence, it’s risk of fracture?
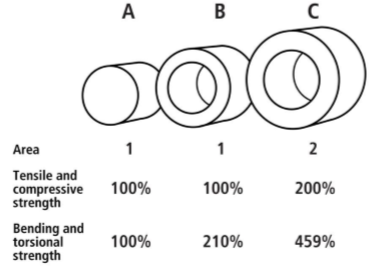
The strength of bone is determined by a combination of its density, size, and shape. When we consider strength, we can think of this as a resistance to being squashed (compressive) or pulled (tensile), or resistance to bending and twisting (torsion). Bones in our body experience ALL of these loading conditions. Adding bone mass is important for strength, but it is equally important to know where the mass is located. For a long bone, the cross-sectional area of the bone and the thickness of the cortical bone have a huge impact on the strength of the bone. Figure 4 below illustrates this. Cylinders A and B have the same unit area of bone (1 square unit) and the same resistance to tensile and compressive forces. However, cylinder B has distributed the bone to the outside and has a hollow center. This results in much stronger resistance to bending and torsional forces. Cylinder C has twice the mass (or area in the cross-section; 2 square units) and also a greater moment of inertia (cross-section diameter). The added mass results in a proportional increase in tensile and compressive strength. By contrast, because the moment of inertia is to the 4th power, the bending and torsional strengths become exponentially greater from bar A to C.
Figure 4. The influence of bone cross-sectional area and size on strength (from https://teambone.com/education-basic/biomechanics-of-bone/).
During growth and development, if we place large bending and torsional loads on our bones, they respond by growing in cross-sectional area. This change in morphology during growth and development stays with us for the rest of our lives (Warden et al., 2014a), so it is extremely important to place large loads on the growing skeleton, to ensure strong bones in our aging years.
Can we predict bone density?
The non-linear relationship between bone density and the loading history means that activity level, body weight, and exercise alone cannot be used as independent variables to correlate with bone density. In order to develop a successful exercise study and predict the changes in bone density, one must carefully quantify the daily loading history and have accurate knowledge of the current bone health.
What are the important mechanical loads that cause bone remodeling?
For most people, the daily history of the ground reaction forces, which account for both body weight and activity level, are the principal source of external forces on the body. The magnitudes of the joint contact forces (which are the forces that are directly applied to the ends of our bones) are related to the magnitude of the ground reaction force and the muscle forces responsible for producing segmental movement. Muscle forces really dominate contact forces, so ideally we would have wearable sensors to tell us what muscle forces cause motion. However, since we cannot easily implant sensors into muscles, we rely on external measures, such as the ground reaction force, or impact experienced from accelerometers, as a relative measurement of the forces applied to the skeleton. We know that elite swimmers and cyclists are at risk of osteopenia or even osteoporosis because they don't experience large impact loads.
Can we mitigate bone loss due to aging?
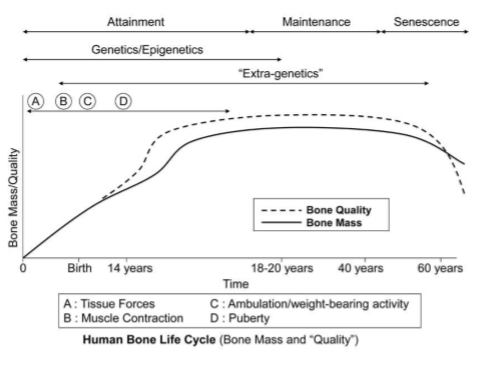
Bone loss can occur at ~0.3% per year after the age of 30yrs. This can be mitigated by physical activity and it only takes a small number of cycles or bone cells to respond. So maintenance of bone is achieved without too much commitment in terms of physical activity! The figure below shows a summary of the human bone life cycle. Early in life, as the skeleton is growing, we see large amounts of bone formation, which is influenced and regulated by mechanical loads (even in utero). After the skeleton has matured, you see little bone mass added. The ‘quality’ of bone here refers to the structural strength, as noted above, which takes into account the size and shape of the bone, not just its density. Note how the quality of bone can be enhanced during growth and development, beyond just the added mass. This is in response to mechanical loads and the additional strength gained from altering the cross-sectional area of bone is maintained throughout life (Warden et al., 2014a).
Figure 5. The influence of aging on bone mass/quality (from https://teambone.com/education-basic/biomechanics-of-bone/).
How long are you allowing bone cells to "recharge" after a dose of loading?
It’s not so much the bone cells recharging, but the repair and maintenance of bone which is necessary. There comes a point in time where additional loading is not necessary to induce a positive remodeling from the bone. There is no solid evidence in the literature that gives an optimal loading regime for an individual. This is partly because; a) everyone is different in terms of our load history, tissue strength, and biological response, and b) we have not had the tools to measure total load exposure before.
Does the magnitude of the load or length of session impact recovery time more?
The IMU bone stimulus metric is useful, as it accounts for both the magnitude and the number of cycles and it should be the main guide for you to decide how much stimulus is enough for the bone. You can achieve the same stimulus in a few different ways. We believe that for healthy tissue, the bone likes a high strain rate and responds more to a high strain rate. However, for a pathological tissue, a paradigm of reduced loading may be preferable.
IMeasureU Support
Comments